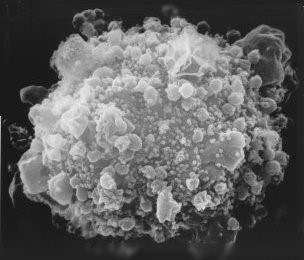
Progress in treating the AIDS / HIV epidemic has been made, but there is still no cure, and new generations are being infected.
SDG Goal 3.3 is about ending several important global epidemics (including AIDS) by 2030. AIDS / HIV is a relatively young epidemic globally. Tylleskär spoke of the first cast of paediatric transmission described in the Lancet in 1988, only 30 years ago. Today, while being HIV+ is no longer the death sentence it was 30 years ago, there is still no cure and speakers at NTNU’s Global Health Day 2018 talked about today’s situation with new generations of people living with the HIV infection.
A key component of SDG 3.3 is prevention
Tylleskär spoke of the second wave of the epidemic – the children born to HIV+ mothers. Tylleskär underlines that HIV is not a highly effective virus – as many as 2/3 of children born to HIV+ mothers do not become infected. However, the global burden new HIV+ generations is tragic, costly and needs to be addressed.
Infants can be infected at several stages: before delivery (5-10%, with the risk increasing as the placenta ages); during delivery (10-20%); and after delivery (10-20%). Antiretroviral treatments (ART) involving the combination or at least 3 drugs have been successful as suppressing virus replication and have ensured that for the most part, mothers on effective HIV treatment do not pass on the virus to their babies before or during birth.
Breast-feeding challenges
The WHO advocates exclusive breastfeeding up to 6 months of age, continued breastfeeding along with appropriate complementary foods up to 2 years of age or beyond. But what if HIV- babies can become infected by breast milk from their HIV+ mothers?
Tylleskär and colleges noted the effect of providing babies of HIV+ mothers with formula milk: undernourished infants with increased morbidity and mortality due to diarrhoeal disease, respiratory disease and other infections.
Why is breast milk ineffective in spite of maternal treatment?
- mothers do not take their ART regularly after pregnancy
- ART stops HIV virus replication, but does not destroy any virus reservoirs that may remain in the body
- virus particles from reservoirs may be shed in breast milk
Preventative measures
Where possible, current WHO routines are ART for HIV+ mothers and a short course of pre-exposure prophylaxis (PrEP) treatment for infants (6 weeks, 12 in high-risk cases). One of Tylleskär’s PhD candidates, David Rutagwera, questions why the PrEP treatment could not be extended for the whole 6 month exclusive breastfeeding period. Read more.
However, the best prevention, underlines Tylleskär, is to stop the acquisition of HIV in the first place. This requires informing and educating young men and women about safe sex norms and behaviours to stop virus transmission.

